No matter what type of tooth pain you are experiencing, one thing is certain; it is one of the worst types of pain you can ever experience, more so when it pops out of nowhere on a Saturday at 2am in the morning! Good news is that there are ways you can manage most types of dental pain on your own, especially when expert dental help is not available.
Managing Dental Pain
Management of different types of dental pains involves diagnosing and treating the underlying issue. While complex issues such as injuries and infections require expert dental help, many dental problems that cause pain can be managed easily at home. There are some instances where tooth pain can result after having a dental treatment such as dental implants, or after recently having Invisalign fitted, if this is the case please speak to your dentist about this treatment.
One of the most common causes of dental pain is wisdom tooth extraction. Let us look at how we can manage wisdom tooth pain.
How to Stop Wisdom Tooth Pain?
Pain associated with a wisdom tooth can arise due to various reasons. First, it can occur if there is tooth decay, making the tooth sensitive to hot or cold foods. Secondly, wisdom tooth pain can occur due to pericoronitis, a condition in which the soft tissues around an impacted wisdom tooth get inflamed. Another painful situation can arise following the removal of a wisdom tooth.
In case you are having pain and swelling around one of your wisdom, then it may be because of pericoronitis. Management of this condition involves maintaining good oral health, taking painkillers to reduce the pain, and using icepacks to reduce the inflammation.
If the underlying cause of pain is due to inflammation then you can manage this situation with pain relievers, warm saline rinses, and icepack application around the region to minimize the inflammation. You can also apply oil of cloves around the tooth with a cotton ball to ease the pain, as it is a natural pain reliever.
Why Are My Gums Painful and Swollen?
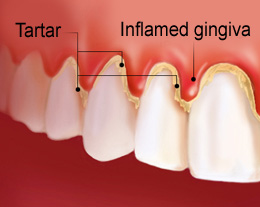
Gums tend to become painful and appear swollen when they have underlying inflammation, a condition clinically known as gingivitis.
Clinically, gingivitis appears as swollen, reddish, and sore gums that tend to bleed easily while eating or brushing. Gingivitis can be easily managed with strict oral hygiene maintenance, and professional teeth cleaning if required.
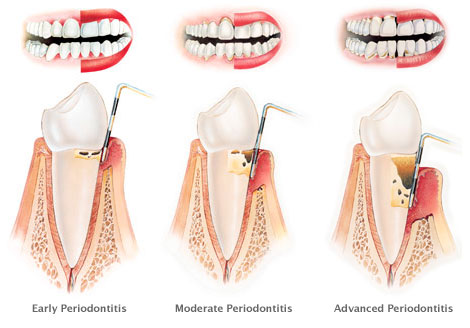
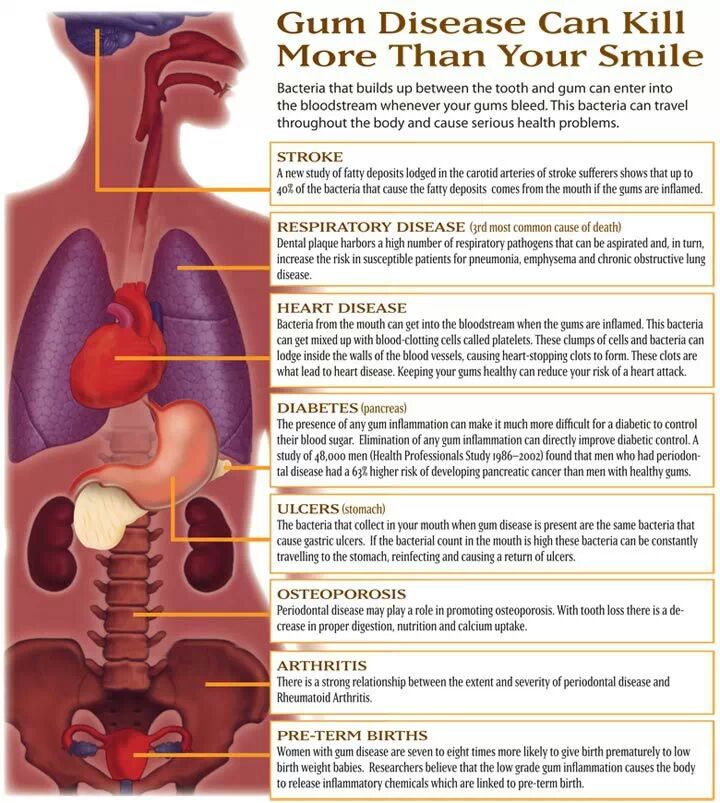
If gingivitis is not treated timely, the inflammation can extend into the tissues that attach our gums to the teeth and the jawbone. This condition called periodontitis causes widespread destruction of the gum tissues, the bone, and the tissues supporting the teeth. As a result, the teeth become mobile if treatment is ignored for a prolonged duration.
Tooth Pain Months or Years After Root Canal
Toothache that occurs a few months or years after a root canal procedure can arise due to a variety of reasons. It may because of incomplete cleaning and disinfection of the tooth’s interior (the root canals), leaving behind bacteria that grow inside the root canals and cause future re-infection.
Another possible reason could be a missed accessory root canal – an extra root canal that is not normally found in that tooth – and is difficult to find. A missed root canal can lead to future re-infection, which is even harder to treat.
How do you Stop Toothache at Home?
When it comes to treating a toothache at home, there are several options you can utilize:
- Pain Medication – pain-relieving medication not only helps in subsiding pain associated with a wisdom tooth or a sinus infection, but it is also helpful in reducing inflammation in the region.
- Icepacks – icepacks help minimize inflammation and swelling at the site of the infection.
- Natural Remedy – one of the best home remedies for stopping wisdom toothache is clove oil. Place a drop of clove oil on a cotton ball and apply it around the infected tooth. You will feel a significant reduction in your pain within 20 minutes of application of this home remedy.
Throbbing Tooth Pain That Comes and Goes, what is The Cause?
If you are having transient, throbbing pain in one of your teeth, it may be a sign of an underlying tooth abscess. An abscess refers to the collection of pus around infected teeth and gums. During the initial stages, the pain of an abscessed tooth can be managed with painkillers. However, in its advanced stages, the pain becomes unbearable, and the only option is to seek expert help immediately. An untreated abscess around the upper molar teeth can also lead to a sinus infection.
While the methods mentioned above are effective relieving wisdom tooth pain, these provide only temporary relief. Once your pain starts to subside, and you feel better, you must immediately book an appointment with your dentist so that the underlying cause of the pain can be diagnosed and treated accordingly.