What are the causes of gum disease?
Gingivitis or Pyria, commonly known as gum disease is an inflammation of the soft tissue area (gum) which surrounds your teeth.
Throughout the day a thin layer called biofilm forms over your teeth, this is known as plaque. This is a sticky and natural layer made up primarily of bacteria. As these bacteria in plaque feed on the sugar, you ingest they excrete acid and it is this acid which causes tooth decay.
When you clean your teeth you will be removing this biofilm layer but if the film is not removed adequately enough then it can begin to harden, particularly in between teeth where it’s difficult to clean. As it hardens it turns into a thick cream coloured layer called tartar.
This tartar can then irritate the gums whilst also giving the bacteria a really good place to read and hide.
This inflammation of the gums, caused by the buildup of tartar then turns into gum disease.
How to catch gum disease?
What are the symptoms of gum disease?
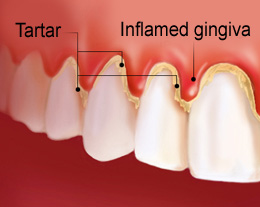
- Gums become red, puffy and inflamed. Typically they will look red and swollen.
- Bleeding can occur, initially only on vigorous brushing or when using an interdental floss or stick.
- Gums can then begin to bleed spontaneously as the gingivitis progresses.
What is periodontal disease?
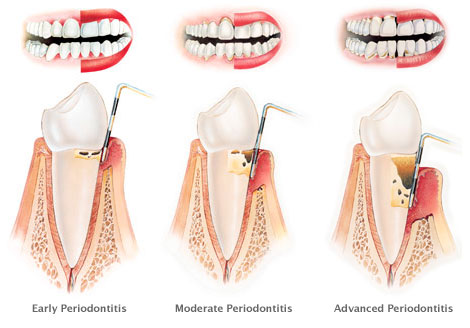
If gum disease is left untreated it can then turn into the more serious periodontal disease. This is where the layer surrounding the root of your tooth becomes inflamed and infected. Gingivitis is an inflammation of the gum, the part of the mouth you can see, periodontitis is an inflammation underneath the gum around the bone, the part of the mouth you can’t see.
Periodontal disease, because it affects the support around the tooth and root if left unchecked can ultimately lead to tooth loss, so it should be treated as a serious condition.
What are the symptoms of periodontal disease?
If you have periodontal disease then you will almost certainly have all of the signs and symptoms of gum disease, in addition, you may also have:
- Gums which are pulling away from your teeth making your teeth look longer.
- Loose or wobbly teeth.
- Puss coming up between your gums and teeth.
- Continuous bad breath.
- Pain in your teeth caused by the pressure of the infection.
What is black gum disease?
- Smoking. Smokers black gums are known as melanosis, this is because there are cells in your gums called melanocytes, nicotine can stimulate these cells to produce more melanin than normal and this gives the dark black appearance on the gums.
- Some medications. Some treatments for chlamydia or acne can result in a side-effect of discolouration of the gums. There are often alternatives so speak to your medical practitioner if you feel this is the cause.
- Old silver fillings. Amalgam (Silver) fillings are extremely dark by nature, looking very black and grey. As you age you may find that the outside of your teeth where you have a filling wears down and becomes thinner, as this happens the amalgam filling can show through. If the amalgam is closed your gum it can give a grey/black appearance to the gum.
- SEVERE gum disease. In some instances of severe gum disease the soft tissue can actually die. This necrosis, sometimes called trench mouth then gives the black appearance. It is often accompanied by extreme bad breath, mouth ulcers, and bleeding gums.
- Hyperpigmentation caused by Addison’s disease. This is a condition which affects the adrenal glands, its symptoms include tiredness, lack of appetite, weak muscles and thirst. The condition has a side-effect that hyperpigmentation occurs in parts of the body and the gums can appear darkened or black.
How can gingivitis be reversed?
How can periodontitis be reversed?
Non-surgical intervention.
Surgical intervention.
- Pocket reduction – this is where the soft tissue around the infected area is gently lifted away, the underlying bone and root can then be extensively cleaned. The gum can then be stitched back into place.
- Soft tissue grafting – if there has been extensive loss of soft tissue (gums) a craft can be taken, often from the roof of your mouth, and used to replace the soft tissue around your teeth.
- Bone grafting – if the periodontitis has infected so much bone the bone has been lost then grafting from either your own bone or synthetic bone can be used to rebuild the area around your teeth.

